Are you a nursing mother struggling to overcome mastitis? Look no further! This article will explore practical strategies to help you overcome this common breastfeeding challenge. Mastitis is an inflammation of the breast tissue that can cause pain, swelling, and flu-like symptoms. It often occurs when milk becomes trapped in the breast, leading to infection.
We understand the importance of finding relief and providing the best care for your baby. That’s why we have gathered expert advice and practical tips to help you overcome mastitis. From proper breastfeeding techniques and frequent nursing to using warm compresses and taking antibiotics if necessary, we will provide you with a comprehensive guide to managing mastitis.
Every mother deserves support and guidance on her breastfeeding journey. Our mission is to empower you with the knowledge and resources to make informed decisions about your and your baby’s health. Join us as we delve into proven strategies for overcoming mastitis and regain your breastfeeding confidence.
What Is Mastitis And Its Causes?
Mastitis is a common condition that affects breastfeeding mothers. It is an inflammation of the breast tissue, usually caused by a bacterial infection. The infection occurs when bacteria enter the breast through a cracked or sore nipple. Other causes of mastitis include milk duct blockage, poor breastfeeding technique, and a weakened immune system.
Mastitis can be painful and uncomfortable. It often presents symptoms such as breast tenderness, redness, swelling, and warmth. Some women may also experience flu-like symptoms such as fever, chills, and body aches. If left untreated, mastitis can lead to the formation of an abscess, which may require surgical drainage.
To prevent mastitis, it’s essential to maintain good breast hygiene and ensure proper latch and positioning during breastfeeding. Avoiding tight-fitting or underwire bras that may restrict milk flow is also recommended. The following section will discuss the importance of early detection and treatment.
Symptoms And Signs Of Mastitis
Recognizing the symptoms and signs of mastitis is crucial for early detection and prompt treatment. Breast pain, swelling, warmth, and redness are the most common symptoms. You may also notice a lump or thickening in the affected area. Additionally, mastitis often presents with flu-like symptoms such as fever, chills, fatigue, and body aches.
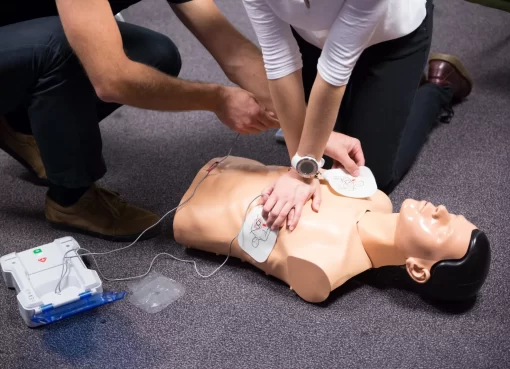
If you experience these symptoms, seeking medical attention promptly is essential. Early treatment can help prevent complications and promote faster recovery. Your healthcare provider will likely perform a physical examination and may recommend additional tests, such as a breast ultrasound or a breast milk culture, to confirm the diagnosis.
The following section will discuss the importance of early detection and treatment in managing mastitis effectively.
The Importance Of Early Detection And Treatment
Early detection and prompt treatment are crucial in managing mastitis effectively. If left untreated, mastitis can worsen and lead to complications such as breast abscess formation. By recognizing the early signs of mastitis and seeking medical help, you can minimize the impact on your breastfeeding journey.
When you notice symptoms of mastitis, it’s essential to rest and take care of yourself. Get plenty of rest and fluids to help your body fight the infection. Warm compresses to the affected breast can help relieve pain and promote milk flow. You can also gently massage the breast to help unclog milk ducts.
It’s recommended to continue breastfeeding or expressing milk regularly, even if it’s uncomfortable. Breastfeeding helps drain the affected breast and prevents milk from accumulating, reducing the risk of further infection. If breastfeeding is too painful, you can use a breast pump to express milk.
Sometimes, your healthcare provider may prescribe antibiotics to treat the infection. It’s essential to take the entire course of antibiotics as prescribed, even if you start feeling better. This will ensure that the infection is completely cleared and prevent the development of antibiotic-resistant bacteria.
Effective Strategies For Preventing Mastitis
Preventing mastitis is possible with the right strategies and precautions. Here are some effective methods to help you reduce the risk of developing mastitis:
- Maintaining good breast hygiene: Clean your breasts and nipples before and after breastfeeding. Avoid using harsh soaps or lotions that may dry out the skin.
- Ensuring proper latch and positioning: Ensure your baby is correctly latching onto the breast to ensure efficient milk transfer and prevent nipple damage. Seek help from a lactation consultant if you need clarification.
- Avoid tight-fitting bras: Opt for comfortable, well-fitting bras that provide adequate support without constricting milk flow. Consider using nursing bras that allow easy access for breastfeeding.
- Emptying your breasts regularly: Breastfeed or express milk regularly to prevent milk from accumulating and clogging milk ducts. If you miss a feeding, use a breast pump to maintain milk supply and to avoid engorgement.
Managing stress and fatigue: Take care of yourself by getting enough rest, eating a healthy diet, and managing stress. Stress and exhaustion can weaken the immune system, making you more susceptible to infections.
Incorporating these strategies into your breastfeeding routine can lower the risk of developing mastitis and enjoy a smoother breastfeeding experience. The next section will discuss proper breastfeeding techniques to prevent mastitis.
Proper Breastfeeding Techniques To Prevent Mastitis
Using proper breastfeeding techniques can help prevent mastitis and promote optimal milk flow. Here are some tips to ensure a successful breastfeeding experience:
- Ensure a deep latch: Ensure your baby’s mouth covers a large portion of the areola, not just the nipple. This helps prevent nipple damage and ensures effective milk transfer.
- Positioning: Find a comfortable position that allows you and your baby to relax during breastfeeding. Experiment with different positions, such as the cradle hold, football hold, or side-lying position, to find what works best for you.
- Break the latch correctly: To avoid nipple damage, gently insert your finger into the corner of your baby’s mouth to break the suction before removing the breast.
- Feed on demand: Respond to your baby’s hunger cues and feed on demand. This helps prevent engorgement and ensures that your breasts are emptied regularly.
- Alternate breastfeeding positions: Switching positions during breastfeeding helps ensure that all areas of the breast are drained thoroughly. Try different positions during each feeding session.
By following these proper breastfeeding techniques, you can minimize the risk of developing mastitis and promote a comfortable and successful breastfeeding journey. The next section will explore natural remedies for relieving mastitis symptoms.
Natural Remedies For Relieving Mastitis Symptoms
In addition to medical treatments, several natural remedies can help relieve mastitis symptoms and promote healing. Here are some natural remedies you can try:
- Warm compresses: Applying warm compresses to the affected breast can help reduce pain and inflammation. Soak a clean washcloth in warm water and place it on the breast for 10-15 minutes daily.
- Cold compresses: Cold compresses can help reduce swelling and discomfort. Use a cold pack or a bag of frozen peas wrapped in a thin cloth and apply it to the affected breast for 10-15 minutes.
- Cabbage leaves: Some women find relief by placing chilled cabbage leaves on the affected breast. The cabbage’s coolness and anti-inflammatory properties can help reduce pain and swelling.
- Epsom salt soak: Adding Epsom salt to warm water and soaking your breasts for 10-15 minutes can help reduce inflammation and promote healing. Be sure to rinse your breasts thoroughly after the soak.
- Herbal remedies: Some herbs, such as calendula and marshmallow root, have anti-inflammatory properties and can help relieve mastitis symptoms. Consult a healthcare professional or a lactation consultant before using any herbal remedies.
It’s important to note that natural remedies should complement and not replace medical treatments. If your symptoms worsen or persist despite using natural remedies, consult your healthcare provider for further evaluation and treatment. In the next section, we will discuss the role of antibiotics in treating mastitis.
The Role Of Antibiotics In Treating Mastitis
In some cases, antibiotics may be necessary to treat mastitis, especially if the infection is severe or doesn’t improve with home remedies. Antibiotics are prescribed to kill the bacteria causing the disease and prevent it from spreading.
If your healthcare provider prescribes antibiotics, taking them as directed is essential. Follow the recommended dosage and complete the full course of antibiotics even if you start feeling better. This ensures the infection is completely cleared and reduces the risk of developing antibiotic-resistant bacteria.
It’s also important to note that some antibiotics are safe to take while breastfeeding, while others may require you to pause breastfeeding temporarily. Discuss any concerns or questions about antibiotics with your healthcare provider to ensure the best treatment for you and your baby.
In the next section, we will provide information on support and resources for nursing mothers with mastitis.
Support And Resources For Nursing Mothers With Mastitis
Dealing with mastitis can be challenging, both physically and emotionally. It’s essential to seek support and access available resources to help you through this experience. Here are some support options and resources for nursing mothers with mastitis:
- Lactation consultants: Lactation consultants are trained professionals who can provide guidance and support in breastfeeding. They can help you with proper latch and positioning, troubleshooting breastfeeding issues, and managing mastitis.
- Support groups: Joining a support group for breastfeeding mothers can provide a sense of community and understanding. You can share experiences, ask questions, and gain support from other mothers who have gone through or are going through mastitis.
- Online resources: Numerous websites, forums, and blogs are dedicated to breastfeeding and mastitis. These resources can provide valuable information, tips, and support from other nursing mothers.
- Healthcare professionals: For guidance and support, contact your healthcare provider, nurse, or midwife. They can provide medical advice, prescribe treatments, and address any concerns you may have.
Remember, you are not alone in this journey. Reach out for support and utilize available resources to help you overcome mastitis and continue providing the best care for your baby.
When To Seek Medical Help For Mastitis
While most cases of mastitis can be managed at home with proper care and treatment, there are instances when medical help should be sought. Contact your healthcare provider if:
- Your symptoms worsen or don’t improve with home remedies.
- You develop a high fever (above 101°F or 38.3°C).
- You notice pus or blood in your breast milk.
- You experience severe pain or difficulty breastfeeding.
- You develop a breast abscess or a firm, painful lump that doesn’t resolve on its own.
Your healthcare provider will evaluate your symptoms, perform a physical examination, and provide appropriate treatment based on your condition.
Conclusion: Empowering Nursing Mothers To Overcome Mastitis
Mastitis is a common challenge faced by many nursing mothers, but with the right strategies and support, it can be overcome. This article explored effective methods for preventing and managing mastitis, including proper breastfeeding techniques, natural remedies, antibiotics when necessary, and available support and resources.
Remember, taking care of yourself is essential for your and your baby’s well-being. Prioritize rest, practice good breast hygiene, and seek support when needed. With perseverance and the right tools, you can overcome mastitis and continue providing the best care for your little one.